Swelling has long been a concern for physicians and their patients, whether the swelling is due to cancer surgery, orthopedic surgery, trauma, sports injuries, diabetes, venous stasis ulcers, radiation, chronic venous insufficiency or plastic/reconstructive surgery.
What is Lymphedema?
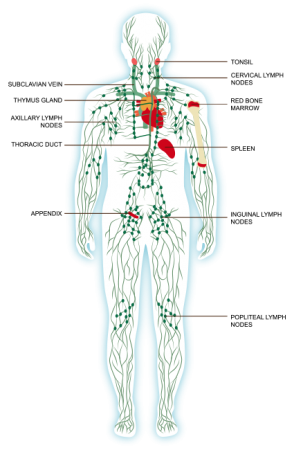
Lymphedema (chronic swelling) occurs when an interruption of lymphatic flow results in the accumulation of lymphatic fluid causing abnormal swelling in the arms, legs, feet, breast, abdomen, neck or head. When lymphatic vessels are impaired, missing, or when lymph nodes are removed, the remaining lymph pathways become congested or blocked. These fluids (waste products) can build up in the connective tissues and becomes thicker and the affected areas feel heavy. This thickening of lymphatic fluid is called fibrosis (hardening of the skin and underlying tissue).